All Posts:
Microplastics: What are they, do they pose a health threat, and what can I do about them?
American Heart Association’s 2025 CPR Guidelines
Do Psychedelics Have a Place in TBI Treatment?
August Is National Immunization Month
Normal Pressure Hydrocephalus
Revolutionizing Accessibility and Affordability in Prosthetics: A Life Care Planning Perspective
Neurodiversity Awareness
The Risks of Using Weight Loss Drugs Without a Prescription

j Microplastics: What are they, do they pose a health threat, and what can I do about them?
By Susan Wirt
If you have listened to any news lately, you have likely heard the term “microplastics (MP).” This seemingly new term has become increasingly more discussed in relation to contaminated water, food sources, and its presence in the human body. MPs are defined as tiny plastic particles, less than 5 mm in size, or about the size of the top of a standard pencil eraser. They can enter the body through inhalation, ingestion, or the skin. In addition to food, beverages, and water, MPs have been identified in cookware, clothing pieces, cosmetics, and personal care products. One recently published study demonstrated that chewing gum, even the plant-based types, results in small amounts of MPs being released into the body, with the greatest “release” occurring within the first eight (8) minutes of chewing (Lowe et al., 2025). Even toothpastes have been found to have significant amounts of MPs (Chengappa et al, 2023).
Current research suggests that the presence of microplastics in the human body has the potential to cause harm through several pathways. Increased inflammation and cellular damage, including DNA damage, are two known ways microplastics negatively impact health. Additionally, larger particles can create intestinal damage by physical friction. Small and large particles can absorb microorganisms, heavy metals, pollutants, and other toxins, introducing these contaminants into the body, a concept considered by many to be the Trojan horse effect.
Although studies on the impact of MPs on human health are relatively new, several have demonstrated negative effects on metabolic, reproductive, digestive, and respiratory health, as well as on some cancers. Although plastics surround us and are essentially unavoidable, there are a few things we can consider. First, we must support increased research regarding MPs, including improved detection tools, investigation of the toxic effects on health of humans and wildlife, identification of new materials, including biodegradable plastics, and improving public awareness and management of plastic products. Be aware that levels of MPs are higher in packaged water and other beverages. The same is true for plastic food containers and utensils (Voelker, 2026). Microwaveable plastic food containers leach MPs into the foods stored and cooked in them. This suggests we should avoid purchasing foods packed in plastic pouches and also avoid microwaving in any plastic containers. Consider reusable stainless steel water bottles.
Finally, MPs have been found in all aquatic areas, including fresh and salt water. Therefore, it is not surprising to learn that your “healthy” meal of fish or seafood (fish products) is also contaminated with MPS. However, there is insufficient data to determine the amount of MPs we ingest from consuming fish products, and the risks to human health remain unknown.
References
Ashwin KRN, & Srimuruganandam B. (2025). Bakelite to microplastics contamination: A comprehensive review on microplastics sources, distribution and their characteristic existence in environment. Emerging Contaminants, 11(1), 100454.
Chengappa,S., Rao, A., Jodalli, P., & Senoy, K. (2023). Microplastic content of over-the-counter toothpastes - a systematic review. F1000Research, 12, 390. source
Kovacs, J., Zrubka, Z., & Garai-Fodor, M.(2025 May 24). Microplastics and their human health effects - Systematic review of systematic reviews in research of microplastics. In 2025 IEEE 19th International Symposium on Applied Computational Intelligence and Informatics (SACI), Timisoara, Romania. source
Lowe, L., Leonard, J. & Mohanty, S. (2025). Ingestion of microplastics during gum chewing consumption. Journal of Hazardous Materials Letters, 6. source
Mahalingaiah, S., Nadeau, K. C., & Christiani, D. C. (2025). Microplastics and human health. Journal of the American Medical Association, 334(21), 1941–1942. source
Voelker, R. (2026). What are microplastics? Journal of the American Medical Association. source
Zhao, S, Yao, L., Zhu, L., Dong, J. LeBlanc, G., & An, L. (2025). Growing concern over ingested microplastics in humans. Carbon Research, 4(1). source

j American Heart Association’s CPR Guidelines
By Susan Wirt
Are you certified in CPR? Consider this:
Cardiac arrest is a life-threatening condition that affects people across all demographics—regardless of age, gender, race, geographic location, or socioeconomic status. The consequences are severe, with significant morbidity and mortality rates. While we have witnessed some improvements in survival rates, there remains a pressing need for further action. In 2024, approximately 263,711 cases of out-of-hospital cardiac arrests (OHCA) were managed by emergency medical services (EMS). Alarmingly, the survival rate to hospital discharge for those treated by EMS was just 10.5%. However, the survival rate jumps to 13% when bystanders witness the event and initiate CPR. Despite these numbers, only 42% of adults suffering from an OHCA received the life-saving assistance of bystander CPR. In response to these challenges, the American Heart Association (AHA) released updated CPR guidelines in October.
Among the 760 recommendations presented, only 11 are grounded in the highest-quality evidence from randomized clinical trials (RCTs). These guidelines comprehensively cover both in-hospital cardiac arrest (IHCA) and out-of-hospital cardiac arrest (OHCA) for adults, children, and neonates. They also delve into post-cardiac arrest care, focusing on minimizing neurological damage and organ dysfunction, while identifying correctable causes of cardiac arrest. Early, high-quality CPR and defibrillation are the most vital actions linked to improved outcomes for adult cardiac arrest patients. Notably, the new guidelines also include essential training on opioid overdose management for cases of opioid-associated OHCA, underlining our commitment to saving lives in this growing crisis.
Several of the new guidelines are summarized here:
CPR standards for everyone:
AHA recommends more CPR training in schools, workplaces, and public events to increase the chances that someone nearby can help before EMTs. CPR training should start with children 12 years of age or older to increase willingness and self-confidence in later years.
Fairness and access:
AHA identified the need to reduce gaps in care due to location, race, income, or other social factors, recommending increased availability of instructor-led training in communities. Media campaigns should be considered to promote the importance of CPR. Communities may want to consider implementing policies that require CPR certification for the general public.
Compression-to-ventilation ratio:
CPR cycles of 30 chest compressions followed by two (2) breaths (as opposed to continuous compression)allow the rescuer to check for adequate ventilation.
New steps for choking:
Five back blows and five abdominal thrusts, repeating until the blockage clears. For babies, give five back blows and five chest thrusts instead.
Opioid emergencies:
Start CPR right away and give naloxone (Narcan) if available (don’t delay CPR while trying to figure it out). Communities should not only expand naloxone distribution programs but also consider public policies that allow for possession, use, and immunity from civil and criminal liability for the good-faith administration of naloxone by lay rescuers.
Kids need fast breathing support:
Children usually go into cardiac arrest because of breathing problems rather than heart disease, thus quick rescue breaths or CPR are critical.
Hard and fast compressions are still key:
High-quality chest compressions are the most important part of adult CPR.
Stay on the scene:
Emergency teams are advised to focus on CPR where the person collapses (rather than rushing them to the hospital). Moving someone too soon can reduce survival chances.
Visit https://cpr.heart.org/en/resuscitation-science/cpr-and-ecc-guidelines for a full copy of the guidelines.
j Do Psychedelics Have a Place in TBI Treatment?
By Susan Wirt
A recent article in Science (2025) examined the use of psychedelic drugs, such as ayahuasca, by professional athletes who have sustained brain injuries from repeated concussions. Buffalo Bills safety Jordan Poyer, retired Raiders guard Robert Gallery, and San Francisco 49ers guard Jon Feliciano were interviewed for the piece. Each discussed how the use of psychedelic substances has had a positive impact on their personal lives off the field. A deeper review of medical literature highlighted positive findings when certain psychedelic drugs are used in treating traumatic brain injury (TBI). These studies have included both military veterans and athletes; however, they have primarily focused on psychological outcomes rather than biological or physiological mechanisms of action.
The term psychedelics refers to a wide array of chemical compounds that “induce distinctly ‘mystical-type’ experiences” (Acero et al., 2023). Robust research into the therapeutic potential of these compounds came to a halt with the passage of the Controlled Substances Act in 1970, which classified them as Schedule I—reserved for the most dangerous and abusable illegal substances. In recent years, shifting public opinion has sparked renewed scientific interest in psychedelics. Despite this resurgence, little is known about their mechanisms of action, aside from their ability to induce “transformative and personally meaningful experiences that correlate with positive behavioral changes” (p. 2).
Neuroplasticity—the ability of brain cells (neurons) to form new connections—is the primary mechanism for functional recovery after TBI or stroke. Some psychedelics are believed to promote neuroplasticity through several mechanisms. For example, harmine is thought to have neuroprotective effects by reducing inflammatory reactions in neurons. Additionally, psilocybin and dimethyltryptamine (DMT) have been shown to improve neuronal survival. These findings suggest that psychedelics may play a role in enhancing neuroplasticity.
Unfortunately, TBI also predisposes individuals to psychiatric disorders. This may result directly from neuronal damage and/or from the psychological stress that follows a TBI. One study investigated the use of ibogaine, an ancient psychedelic, in treating psychiatric disorders associated with TBI. A small trial of 30 U.S. military special operations forces veterans with a history of TBI found marked improvements in “PTSD severity, depression severity, anxiety, and cognitive performance” after treatment with ibogaine and magnesium (Cherian et al., 2024). Reported results included an 87% reduction in depressive symptom severity and an 83% remission rate (p. 375). However, because this was not a randomized controlled trial—the gold standard in medical research—many questions remain unanswered.
Brody and Siddiqi (2024) used resting-state functional magnetic resonance imaging (fMRI) to compare three groups of military veterans: (1) those with TBI and depressive symptoms, (2) those with TBI but no substantial depressive symptoms, and (3) those with no TBI but depressive symptoms. They concluded that certain affective disorders in individuals with TBI may be pathophysiologically distinct from those in individuals with other mood disorders. Their findings identified unique brain connectivity patterns, which they termed “TBI affective syndrome” (p. 342).
Psychedelic researcher Josh Allen, from Vancouver Island University and the University of Victoria, compares these compounds to “brain fertilizer” due to their ability to promote new neuronal connections. Another researcher, Manesh Girn, a neuroscientist at the University of California, San Francisco, is investigating the use of 5-MeO-DMT, which he believes holds promise for treating cognitive impairment such as emotional dysregulation, impaired decision-making, and other cognitive deficits, including memory, language, and attention (Semley, 2025, p. 8).
The takeaway is clear: research is promising but still limited. More controlled investigations into mechanisms of action, clinical applications, and safe use guidelines are necessary to advance this field—not only for TBI, but for other disorders as well. For more information about psychedelic research studies in the U.S., see: https://pmc.ncbi.nlm.nih.gov/articles/PMC9567237/
References
Acero, V. P., Cribas, E. S., Browne, K. D., Rivellini, O., Burrell, J. C., O’Donnell, J. C., Das, S., & Cullen, D. K. (2023). Bedside to bench:
The outlook for psychedelic research. Frontiers in Pharmacology, 14, 1240295. https://doi.org/10.3389/fphar.2023.1240295
Brody, D. L., & Siddiqi, S. H. (2024). An ancient psychedelic for traumatic brain injury. Nature Medicine, 30, 342–343. https://doi.org/10.1038/s41591-023-02759-w
Cherian, J., et al. (2024). https://pubmed.ncbi.nlm.nih.gov/38518270/
Semley, J. (2025, September 8). Why former NFL all-pros are turning to psychedelics. Wired.
https://www.wired.com/story/can-psychedelics-reduce-traumatic-brain-injury-one-nfl-all-pro-thinks-so/

j August Is National Immunization Month
By Susan Wirt
August is National Immunization Awareness Month, a time to highlight the vital role vaccines play in protecting public health. Healthcare professionals bear a serious responsibility to proactively encourage vaccination, build community trust, and provide clear, evidence-based guidance. Through informed communication and leadership, providers help ensure that individuals and families stay up to date on recommended immunizations.
The Public Health Impact of Vaccines
Immunizations are among the most effective tools in modern medicine, drastically reducing the spread of serious, potentially life-threatening diseases. From infancy through adulthood, vaccines protect both individuals and communities by preventing outbreaks and maintaining herd immunity. Diseases that once caused widespread illness and death—such as polio, measles, and diphtheria—are now rare in many parts of the world due to widespread vaccination efforts.
A History of Scientific Progress
The history of vaccines reflects centuries of scientific advancement. Starting with Edward Jenner’s 1796 smallpox vaccine, continued progress in microbiology and immunology has led to the development of safe and effective vaccines for a broad array of diseases. Programs such as Vaccines for Children have expanded access, preventing millions of hospitalizations and delivering significant healthcare cost savings by immunizing generations of children against preventable illnesses.
According to the National Foundation for Infectious Diseases, vaccination rates for school-age children have dropped by as much ast 6%-18%, depending on the vaccine or the age group. Some of the decline is associated with the fact that many people today did not experience periods of major outbreaks of polio, measles, or mumps. Their understanding of the impact of these outbreaks is limited, and they lack the respect or fear of these childhood diseases.
However, recent CDC reports show that more teens got recommended vaccinations in 2024 than did so in 2023. This trend is the opposite of what’s happening in younger children. This finding suggests that communication between providers, parents, and teens can lead to higher vaccine rates. For some of the diseases targeted by the vaccines on the CDC’s immunization schedule, even the increase in teens getting the shots doesn’t mean the U.S. is at a herd immunity level, the point at which the population as a whole is more generally protected from an illness. For example, to achieve herd immunity for pertussis, 92 to 94 percent of the population needs to be vaccinated. Kindergartners and teen vaccination rates still fall just under the lower threshold for herd immunity. As a result of these below-threshold rates, there were more than 35,000 cases of whooping cough in the US in 2024, while there were only 7,000 in 2023.
Safety, Innovation, and the Role of Healthcare Providers
All vaccines approved for use in the United States undergo extensive testing and ongoing monitoring to ensure safety and efficacy. While minor side effects—like soreness or low-grade fever—are common, serious reactions are exceedingly rare. Clinical data confirm that immunizations prevent millions of disease cases and save countless lives annually.
The recent decision by Health Secretary Robert F. Kennedy Jr. to terminate nearly $500 million in federal funding for 22 mRNA vaccine research projects—including work with leading institutions like the University of Texas Medical Branch (UTMB)- is believed by experts to be a “deeply misguided move.” Public health officials, physicians, nurses, and medical researchers warn that this policy threatens pandemic preparedness and U.S. biodefense, as mRNA vaccines enabled rapid, effective responses during COVID-19 and are being researched for other critical applications, such as cancer and emerging infections. Researchers have labeled the decision irrational and harmful, noting that mRNA platforms can be designed and produced quickly, making them vital against future threats.
Cutting this research not only undermines public health infrastructure but also sends a troubling signal that ideology may take precedence over science. As experts emphasize, abandoning this promising technology puts public safety at risk by weakening the ability to respond swiftly to emergent pathogens. This choice could drive scientists and companies to relocate or shift focus away from the U.S., further eroding research capacity.
Healthcare professionals play a key role not only in administering vaccines but also in reinforcing public confidence—particularly during times when decisions threaten to erode it. Encouraging patients to stay current with their vaccinations and continued advocacy for evidence-based science remains essential to protecting individual health and strengthening public health infrastructure now and in the challenging years ahead.

j Normal Pressure Hydrocephalus
The recent disclosure that legendary musician Billy Joel has been diagnosed with Normal Pressure Hydrocephalus (NPH) has brought renewed attention to a condition that, while relatively rare, is frequently misdiagnosed and underrecognized. For rehabilitation nurses and life care planners, NPH represents a compelling case of how early identification, multidisciplinary coordination, and well-structured follow-up care can significantly impact long-term quality of life.
Understanding the Condition
Normal Pressure Hydrocephalus is a neurological disorder caused by the abnormal accumulation of cerebrospinal fluid (CSF) within the brain's ventricular system. Under normal conditions, CSF circulates around the brain and spinal cord, providing cushioning and nutrient transport, before being reabsorbed by the body. In NPH, the reabsorption process fails, and excess fluid gradually collects, causing the ventricles to enlarge and exert pressure on surrounding brain tissue.
Despite the term "normal pressure," this condition can have serious functional consequences—even though the CSF pressure typically falls within standard ranges on diagnostic testing. This slow and subtle progression makes clinical vigilance critical in older adults, where symptoms are often dismissed as part of the normal aging process.
Hallmark Symptoms
NPH is classically identified by a triad of symptoms, which can vary in severity and presentation:
- Gait Disturbances: Often the earliest sign, individuals may appear to “shuffle,” walk with a wide base, or have difficulty initiating steps. These impairments are frequently misattributed to musculoskeletal disorders such as arthritis or neuropathy.
- Urinary Incontinence: Bladder control may decline over time, beginning with urgency and frequency and progressing in some cases to complete incontinence. This symptom can be particularly distressing and stigmatizing, often triggering secondary psychological concerns.
- Cognitive Decline: Unlike Alzheimer’s Disease, cognitive symptoms in NPH tend to center around executive function—slowness in thinking, difficulty with planning, and emotional flatness or apathy. These changes can be mistaken for depression or generalized cognitive aging.
Implications for Rehab and Planning
For rehabilitation professionals and life care planners, NPH presents a unique opportunity to intervene with effective strategies. The symptoms of NPH can have a profound impact on mobility, self-care, continence, and cognition—domains that are central to quality of life, safety, and independence.
Early and accurate diagnosis is essential. A comprehensive neurological exam should be followed by advanced imaging—typically an MRI, which can clearly show ventricular enlargement. Additional studies like cerebrospinal fluid flow studies or high-volume lumbar punctures may aid in confirming the diagnosis and predicting treatment response.
Treatment and Recovery
The most effective intervention is the surgical placement of a ventriculoperitoneal (VP) shunt, which diverts excess fluid from the brain to another part of the body, typically the abdomen, where it can be absorbed. This relatively routine procedure can lead to significant functional gains, particularly in gait and cognition.
From a rehabilitation nursing standpoint, post-operative care may involve:
- Gait retraining and balance therapy
- Bladder management strategies, including timed voiding or pelvic floor rehab
- Cognitive support and executive function coaching
- Patient and caregiver education, especially regarding shunt care, signs of malfunction, and follow-up protocols
Life Care Planning Considerations
Although NPH is treatable, timing matters. Delayed diagnosis or intervention can result in permanent neurological damage. For life care planners, this underscores the importance of long-term follow-up, appropriate referrals, and integrated care planning.
Plans may include:
- Durable medical equipment for mobility or safety (e.g., walkers, fall prevention systems)
- Structured outpatient therapies (PT/OT/SLP)
- Cognitive or psychological support services
- Incontinence supplies and environmental modifications
- Ongoing neurosurgical and neurologic follow-up
- Contingency planning for potential shunt revisions or complications
Risk Factors and Prevention
While NPH is not fully preventable, several risk factors have been identified, including:
- Hypertension
- Type 2 diabetes
- High cholesterol
- History of traumatic brain injury
As such, primary prevention in the form of cardiovascular health management and fall prevention remains important, especially in older adults.
Final Thoughts
Normal Pressure Hydrocephalus is one of the few reversible causes of dementia and gait disturbance in older adults. With early detection, comprehensive rehabilitation, and thoughtful life care planning, individuals living with NPH can achieve meaningful recovery and maintain independence.
For rehabilitation professionals and care planners, staying attuned to the subtleties of this condition can make all the difference—transforming what might appear to be inevitable decline into a pathway for recovery and renewed function.
Sources:
Hydrocephalus Association – What is NPH?
READ MORE

j Revolutionizing Accessibility and Affordability in Prosthetics: A Life Care Planning Perspective
By Susan Wirt | original article: Tech Briefs
The global reality for individuals with limb loss is stark—90% of amputees lack access to proper prosthetic care. This critical gap in healthcare and rehabilitation prompted LIMBER Prosthetics & Orthotics, Inc. to reimagine prosthetic development through innovative 3D printing technology. By creating structurally sound, one-piece prosthetic limbs, LIMBER is addressing the need for affordable, accessible solutions, significantly benefiting life care planning and rehabilitation case management.
LIMBER’s journey began at the University of California, San Diego, as a research initiative under the guidance of structural engineering professor Falko Kuester. The traditional process of crafting prosthetics, often described as a sculptural art form, involves labor-intensive hand-carving of residual limb models. This method is not only time-consuming and costly but also challenging to scale in underserved regions where prosthetists are scarce.
Recognizing the potential for improvement, Kuester collaborated with Ph.D. student Luca De Vivo Nicoloso. Together with Joshua Pelz, a fellow researcher, and Herb Barrack, a certified prosthetist with over three decades of experience, they founded LIMBER to modernize and streamline prosthetic fabrication.
LIMBER’s approach integrates advanced technology with personalized care, ensuring a seamless and efficient experience for patients and care teams. The process begins with a 3D scan of the patient’s residual limb using an iPhone (model 10 or later). This scan provides an initial geometric model, which is then refined by certified prosthetists who incorporate manual measurements and clinical expertise. This personalized design ensures each prosthetic limb addresses the unique needs of the individual, enhancing comfort, function, and mobility.
The collected data is uploaded to the LIMBER cloud, where it is reviewed and finalized by skilled design technicians and prosthetists. The finalized design is sent to LIMBER’s 3D printing facilities, where the prosthetic is manufactured, post-processed, and shipped to the patient’s care provider for fitting. This streamlined workflow reduces production times significantly, with prosthetics delivered in as little as one to two days in the U.S. and within a week internationally.
LIMBER’s commitment to affordability and accessibility is reflected in its two-pronged business model. In developed countries, the company sells custom prosthetics at competitive prices, while subsidizing services in developing nations to offer discounted or free prosthetics. Collaborating with local institutions, such as rehabilitation centers and community organizations, LIMBER ensures the solutions are culturally relevant and effectively meet the needs of underserved populations. For instance, partnerships with organizations like Rotary Clubs in Mexico demonstrate the company’s dedication to sustainable, community-centered care.
To date, LIMBER has successfully delivered 15 custom-designed prosthetic limbs, achieving a remarkable first-fit success rate. Minor adjustments, such as alignment or socket fit modifications, were easily resolved by prosthetists using LIMBER’s thermoforming technology. This adaptability minimizes disruptions to patient care and exemplifies the company’s focus on practical, patient-friendly solutions
LIMBER’s technology holds immense promise for life care planning and rehabilitation case management, offering a cost-effective, scalable solution to prosthetic care. By reducing production costs and enabling faster delivery, LIMBER empowers case managers and healthcare providers to support patients with timely, high-quality prosthetics that improve their quality of life.
With plans to begin selling 3D-printed prosthetic limbs in the U.S. in early 2024, LIMBER is poised to transform the landscape of prosthetic care, bridging the gap between innovation and accessibility for patients worldwide.

j Neurodiversity Awareness
By Susan Wirt | original article: Newswise
In today’s healthcare landscape, the concept of neurodiversity has become increasingly important, influencing how we approach long-term care and support for individuals with cognitive and developmental differences. A poignant reminder of this shift occurred during the Democratic National Convention, when vice-presidential candidate Tim Walz shared the stage with his son, Gus, who lives with a nonverbal learning disorder and ADHD. This heartfelt moment touched the nation and sparked critical conversations about how society can better support people with neurodivergent conditions.
The Walz family’s openness about Gus’s neurodiversity has been a source of inspiration for many, shining a light on the importance of personalized, compassionate care. Neurodivergent individuals—those with conditions such as autism, ADHD, or learning disorders—often require tailored care plans that address their unique needs while recognizing their strengths. This approach ensures that their support systems, whether medical, educational, or social, are designed to promote independence, improve quality of life, and foster inclusion.
Creating comprehensive, individualized care strategies is key to helping neurodivergent individuals thrive. By understanding each person’s specific challenges, healthcare professionals can collaborate with families, educators, and therapists to develop support systems that offer meaningful resources—from specialized therapies to assistive technologies and educational accommodations. These strategies go beyond addressing medical needs; they focus on building a foundation for long-term success and fulfillment.
Healthcare professionals play a crucial role in advocating for individuals with neurodivergent conditions, ensuring they receive the appropriate therapies, medical care, and services to meet their unique needs. Navigating healthcare systems, coordinating care across various disciplines, and connecting families with the right resources are all essential in helping individuals achieve their full potential. It’s about bridging gaps between medical care, social support, and education, allowing individuals and their families to feel empowered and supported.
The increased awareness of neurodiversity, highlighted by moments like the Walz family’s story, emphasizes the growing need for inclusive and personalized care. As these conversations move further into the mainstream, the healthcare community must continue to advocate for changes that support individuals with neurological differences.
By embracing neurodiversity and recognizing the value of personalized care, we are taking important steps toward a future where every individual, regardless of developmental or cognitive differences, has access to the opportunities and tools they need to succeed. This shift toward understanding and supporting neurodiversity is essential to ensuring that all individuals receive the compassionate, individualized care they deserve.
j The Risks of Using Weight Loss Drugs Without a Prescription
By Susan Wirt | original article: Newswise
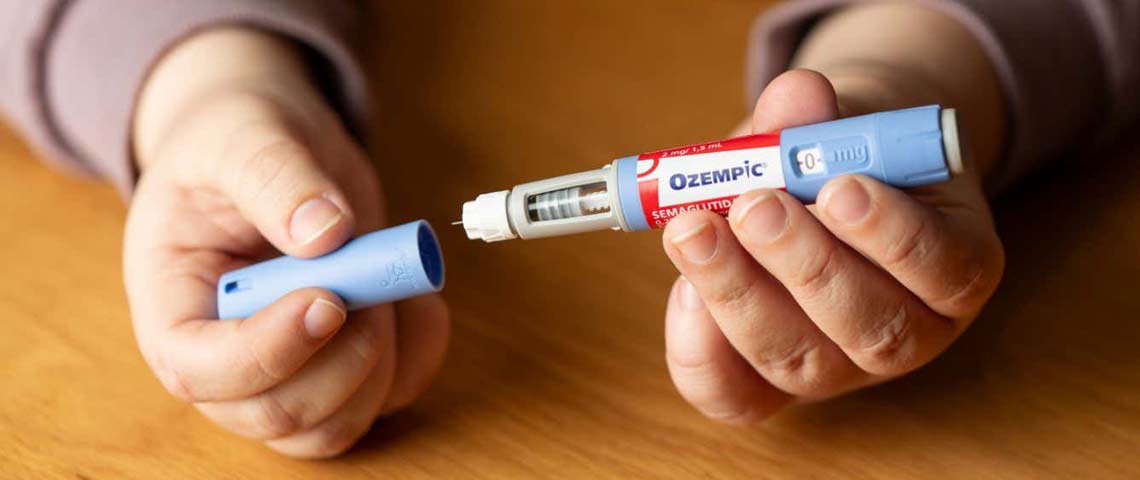
In recent years, injectable weight loss drugs like Ozempic and Wegovy have surged in popularity, offering hope for those struggling with weight management. Initially developed to treat Type 2 diabetes, these medications have also been found to curb appetite and slow digestion, leading to significant weight loss for some individuals. However, their increasing demand, coupled with high costs and limited availability, has driven some people to seek out alternative, often risky, solutions.
A national survey by The Ohio State University Wexner Medical Center revealed that 1 in 4 adults would consider using these medications without consulting a doctor. The motivations range from seeking more affordable options (18%) to facing difficulties accessing the drugs through pharmacies (6%). While the desire for quick results is understandable, bypassing professional medical guidance can pose serious health risks.
Dr. Shengyi Mao, an internal medicine physician at Ohio State, emphasizes the importance of consulting a healthcare provider before starting any medication for weight loss. “Every medication can have risks and side effects,” Dr. Mao notes, and only a trusted medical professional can evaluate an individual’s unique health needs and determine the safest path forward. This is especially true for medications like Ozempic and Wegovy, which, though effective for some, are not without potential complications.
One of the most pressing concerns is the rise of unregulated sources offering counterfeit or compounded versions of these drugs. The FDA has issued warnings about such alternatives, which may contain unapproved active ingredients, posing significant risks to those who use them. These unauthorized versions can lead to unpredictable side effects and undermine the safety that comes with proper medical oversight.
For individuals managing obesity, a complex and chronic condition, seeking out quick fixes can be tempting, but sustainable, long-term health requires a thoughtful, personalized approach. Weight loss should never follow a one-size-fits-all strategy, and decisions about treatment options must take into account each person’s medical history, health goals, and potential risks.
It’s important to remember that while medications like Ozempic and Wegovy can be valuable tools for some, they are just one part of a broader strategy for managing obesity. Addressing weight management holistically—through nutrition, physical activity, behavioral changes, and medical care—provides a safer, more effective path forward.
In this rapidly evolving landscape of weight loss solutions, the guidance of a healthcare provider is essential. A thoughtful, informed approach to care not only protects individuals from unnecessary risks but also sets the stage for long-term success and well-being.
